The Indian Premier League has been suspended for one week amid the ongoing tensions between India and neighbouring Pakistan. Overnight,…
Read More

The Indian Premier League has been suspended for one week amid the ongoing tensions between India and neighbouring Pakistan. Overnight,…
Read More
Former Australia cricketer Stuart MacGill has avoided jail after being found guilty of taking part in the supply of cocaine.…
Read More
Vladimir Putin is leading Russia’s Victory Day commemorations with a parade in Red Square and heightened security after days of…
Read More
BBC / Mike Wendling Mary Simons drove to the church where Pope Leo XIV spent his childhood when she heard…
Read More
Reuters People celebrate at the Cathedral of Saint Mary in Chiclayo, Peru with a banner saying Pople XIV has a…
Read More
The fact that the conclave was over quickly suggests that from the outset, a significant number of the voting cardinals…
Read More
Getty Images The NHS in England is planning “previously unthinkable” cuts to try to balance the books, health bosses say.…
Read More
Yogita Limaye reporting from the Donetsk region BBC Asked about a ceasefire, 26-year-old soldier Max told the BBC “you don’t…
Read More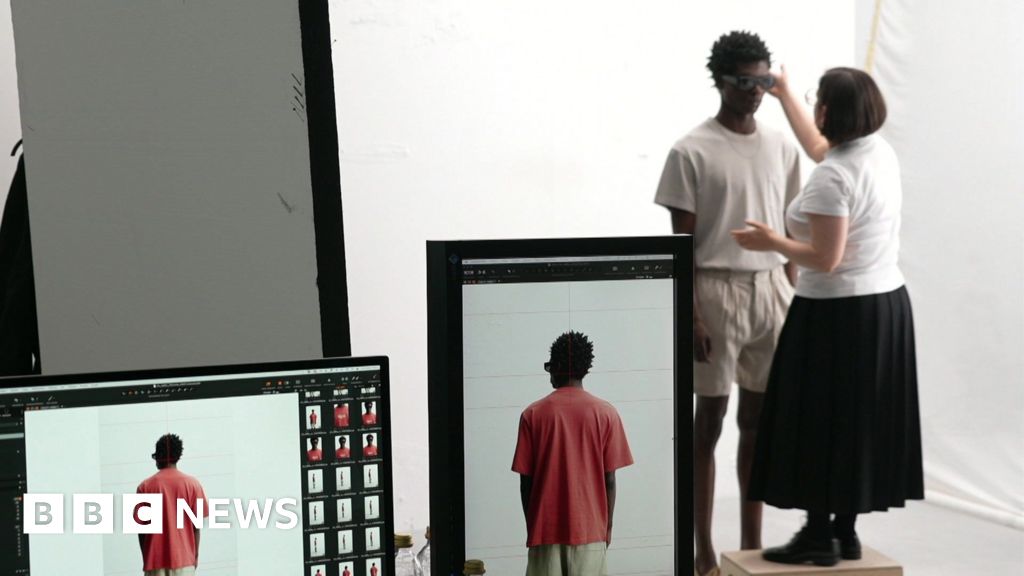
Emma Simpson Business correspondent Watch: BBC given exclusive behind-the-scenes access to Zara’s Spanish headquarters It’s going to be a very…
Read More
8 minutes ago ShareSave ShareSave “U.S. trade deal made by Brexit”, states the Daily Mail which is one of many…
Read More