April 4, 2023 – Lisa McCorkell had a mild bout of COVID-19 in March 2020. Young and healthy, she assumed that she would bounce back quickly. But when her fatigue, shortness of breath, and brain fog persisted, she realized that she most likely had long COVID.
“Back then, we as patients basically coined the term,” she said. While her first primary care provider was sympathetic, they were unsure how to treat her. After her insurance changed, she ended up with a second primary care provider who didn’t take her symptoms seriously. “They dismissed my complaints and told me they were all in my head. I didn’t seek care for a while after that.”
McCorkell’s symptoms improved after her first COVID vaccine in the spring of 2021. She also finally found a new primary care doctor she could trust. But as one of the founders of the Patient-Led Research Collaborative, a group of researchers who study long COVID, she says many doctors still don’t know the hallmark symptoms of the condition or how to treat it.
“There’s still a lack of education on what long COVID is, and the symptoms associated with it,” she said. “Many of the symptoms that occur in long COVID are symptoms of other chronic conditions, such as chronic fatigue syndrome, that are often dismissed. And even if providers believe patients and send them for a workup, many of the routine blood and imaging tests come back normal.”
The term “long COVID” emerged in May 2020. And though the condition was recognized within a few months of the start of the pandemic, doctors weren’t sure how to screen or treat it.
While knowledge has developed since then, primary care doctors are still in a tough spot. They’re often the first providers that patients turn to when they have symptoms of long COVID. But with no standard diagnostic tests, treatment guidelines, standard care recommendations, and a large range of symptoms the condition can produce, doctors may not know what to look for, nor how to help patients.
“There’s no clear algorithm to pick up long COVID – there are no definite blood tests or biomarkers, or specific things to look for on a physical exam,” said Lawrence Purpura, MD, an infectious disease specialist and director of the long COVID clinic at Columbia University Medical Center in New York City. “It’s a complicated disease that can impact every organ system of the body.”
Even so, emerging research has identified a checklist of sorts that doctors should consider when a patient seeks care for what appears to be long COVID. Among them:
- The key systems and organs impacted by the disease
- The most common symptoms
- Useful therapeutic options for symptom management that have been found to help people with long COVID
- The best heathy lifestyle choices that doctors can recommend to help their patients
Here’s a closer look at each of these aspects, based on research and interviews with experts, patients, and doctors.
Key Systems, Organs Impacted
About 10% of people who are infected with COVID-19 go on to have long COVID, according to a recent study that McCorkell helped co-author. But more than 3 years into the pandemic, much about the condition is still a mystery.
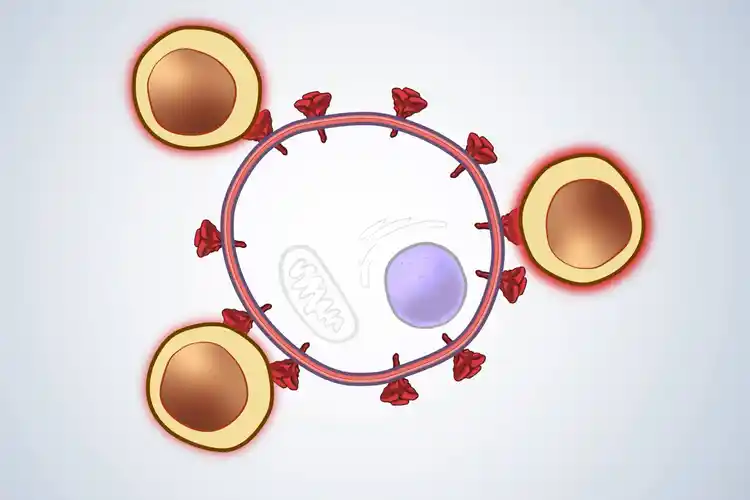
COVID is a unique virus because it can spread far and wide in a patient’s body. A December 2022 study, published in the journal Nature, autopsied 44 people who died of COVID and found that the virus could spread throughout the body and persist, in one case as long as 230 days after symptoms started.
“We know that there are dozens of symptoms across multiple organ systems,” said McCorkell. “That makes it harder for a primary care physician to connect the dots and associate it with COVID.”
A paper published last December in Nature Medicine proposed one way to help guide diagnosis. It divided symptoms into four groups:
- Cardiac and renal issues such as heart palpitations, chest pain, and kidney damage
- Sleep and anxiety problems like insomnia, waking up in the middle of the night, and anxiety
- In the musculoskeletal and nervous systems: musculoskeletal pain, osteoarthritis, and problems with mental skills
- In the digestive and respiratory systems: trouble breathing, asthma, stomach pain, nausea, and vomiting
There were also specific patterns in these groups. People in the first group were more likely to be older, male, have other conditions and to have been infected during the first wave of the COVID pandemic. People in the second group were over 60% female, and were more likely to have had previous allergies or asthma. The third group was also about 60% female, and many of them already had autoimmune conditions such as rheumatoid arthritis. Members of the fourth group – also 60% female – were the least likely of all the groups to have another condition.
This research is helpful, because it gives doctors a better sense of what conditions might make a patient more likely to get long COVID, as well as specific symptoms to look out for, said Steven Flanagan, MD, a physical medicine and rehabilitation specialist at NYU Langone Medical Center who also specializes in treating patients with long COVID.
But the “challenge there, though, for health care providers is that not everyone will fall neatly into one of these categories,” he stressed.
Checklist of Symptoms
Although long COVID can be confusing, doctors say there are several symptoms that appear consistently that primary care providers should look out for, that could flag long COVID. They include:
Post-exertional malaise (PEM). This is different from simply feeling tired. “This term is often conflated with fatigue, but it’s very different,” said David Putrino, PhD, director of rehabilitation innovation at the Mount Sinai Health System in New York City, who says that he sees it in about 90% of patients who come to his long COVID clinic.
PEM is the worsening of symptoms after physical or mental exertion. This usually occurs a day or two after the activity, but it can last for days, and sometimes weeks.
“It’s very different from fatigue, which is just a generalized tiredness, and exercise intolerance, where someone complains of not being able to do their usual workout on the treadmill,” he noted. “People with PEM are able to push through and do what they need to do, and then are hit with symptoms anywhere from 12 to 72 hours later.”
Dysautonomia. This is an umbrella term used to describe a dysfunction of the autonomic nervous system, which regulates bodily functions that you can’t control, like your blood pressure, heart rate, and breathing. This can cause symptoms such as heart palpitations, along with orthostatic intolerance, which means you can’t stand up for long without feeling faint or dizzy.
“In my practice, about 80% of patients meet criteria for dysautonomia,” said Putrino. Other research has found that it’s present in about two-thirds of long COVID patients.
One relatively easy way primary care providers can diagnose dysautonomia is to do the tilt table test. This helps check for postural orthostatic tachycardia syndrome (POTS), one of the most common forms of dysautonomia. During this exam, the patient lies flat on a table. As the head of the table is raised to an almost upright position, their heart rate and blood pressure are measured. Signs of POTS include an abnormal heart rate when you’re upright, as well as a worsening of symptoms.
Exercise intolerance. A 2022 review published in the journal JAMA Network Open analyzed 38 studies on long COVID and exercise and found that patients with the condition had a much harder time doing physical activity. Exercise capacity was reduced to levels that would be expected about a decade later in life, according to study authors.
“This is especially important because it can’t be explained just by deconditioning,” said Purpura. “Sometimes these patients are encouraged to ramp up exercise as a way to help with symptoms, but in these cases, encouraging them to push through can cause post-exertional malaise, which sets patients back and delays recovery.”
While long COVID can cause dozens of symptoms, a paper McCorkell co-authored zeroed in on some of the most common ones:
- Chest pain
- Heart palpitations
- Coughing
- Shortness of breath
- Belly pain
- Nausea
- Problems with mental skills
- Fatigue
- Disordered sleep
- Memory loss
- Ringing in the ears (tinnitus)
- Erectile dysfunction
- Irregular menstruation
- Worsened premenstrual syndrome
While most primary care providers are familiar with some of these long COVID symptoms, they may not be aware of others.
“COVID itself seems to cause hormonal changes that can lead to erection and menstrual cycle problems,” explained Putrino. “But these may not be picked up in a visit if the patient is complaining of other signs of long COVID.”
It’s not just what symptoms are, but when they began to occur, he added.
“Usually, these symptoms either start with the initial COVID infection, or begin sometime within 3 months after the acute COVID infection. That’s why it’s important for people with COVID to take notice of anything unusual that crops up within a month or two after getting sick.”
Can You Prevent Long COVID?
You can’t, but one of the best ways to reduce your risk is to get vaccinated. Getting at least one dose of a COVID vaccine before you test positive for COVID lowers your risk of long COVID by about 35% according to a 2022 study published in Antimicrobial Stewardship & Healthcare Epidemiology. Unvaccinated people who recovered from COVID, and then got a vaccine, lowered their own long COVID risk by 27%.
In addition, a February study published in JAMA Internal Medicine found that women who were infected with COVID were less likely to go on to get long COVID and/or have less debilitating symptoms if they had a healthy lifestyle, which included the following:
- Healthy weight (a BMI between 18.5 and 24.7)
- Never smoker
- Moderate alcohol consumption
- A high-quality diet
- Seven to 9 hours of sleep a night
- At least 150 minutes per week of physical activity
But McCorkell noted that she herself had a healthy pre-infection lifestyle but got long COVID anyway, suggesting these approaches don’t work for everyone.
“I think one reason my symptoms weren’t addressed by primary care physicians for so long is because they looked at me and saw that I was young and healthy, so they dismissed my reports as being all in my head,” she explained. “But we know now anyone can get long COVID, regardless of age, health status, or disease severity. That’s why it’s so important that primary care physicians be able to recognize symptoms.”
https://img.webmd.com/vim/live/webmd/consumer_assets/site_images/logos/webmd/web/webmd-logo-fb.jpg
2023-04-04 19:18:07





