
 BBC
BBCListen to this article on BBC Sounds
Ministers, health staff and the public gathered in London last week for a summit to discuss the 10-year NHS plan in England. It was the final roadshow in a nationwide tour to help set out the strategy the government says will rescue the “broken” NHS, which has a waiting list of nearly 7.5 million patients and public satisfaction of just 21% – a record low.
Not for the first time, moving healthcare away from hospitals and into the community is being touted as a way of treating people better and for less. Research suggests that every £100 spent on community care would otherwise cost £131 for hospital care.
This helps explain why Health Secretary Wes Streeting has promised to turn the NHS into a neighbourhood health service.
Washwood Heath, a community health clinic that was set up in a deprived part of east Birmingham two years ago when the Conservative government was in power, is a living, working example of what this could look like. Here, hospital doctors, GPs, nurses, occupational therapists, council social care teams, mental health professionals and charity staff work under one roof.

The three-story building combines an urgent treatment centre offering some of the services usually provided by hospitals, as well as a diagnostic service (for MRI scans, X rays and ultrasounds), alongside mental health care and wider social support.
In practice, this allows for addressing social problems such as housing issues, alongside treating physical health conditions, plus arranging support for daily tasks such as washing and dressing.
The target is the most frequent users of health services – and the aim is to keep them well and out of hospital.
“We want to work with the 10% of the population that is responsible for 70 to 80% of its use,” explains Richard Kirby, head of Birmingham Community Healthcare NHS Trust, one of the key partners at Washwood Heath. “The NHS cannot meet their needs on its own – it requires partnership working.”
Streeting himself is on board. Speaking to the BBC this week, he said that Washwood was a “pioneering service” and he is firm that the model could “be the future of the NHS”.
However not everyone is convinced. And while few argue against the principle of more care within the community, there are wider questions around just how feasible it is on a bigger scale.
A model system to unblock beds?
In the middle of the clinic, staff gather around five touchscreens, each containing up-to-date information about patients from east Birmingham who are in hospital or making calls to the ambulance service. Their goal is to get these patients discharged from hospital as swiftly as they can – and keep them out.
One way of doing this is by arranging remote monitoring from the ‘virtual wards team’ (which allows doctors to keep an eye on patients who would otherwise have to stay on the wards), as well as ordering equipment such as mobility aids and medicine dispensers to be delivered to their homes.

The team is also automatically alerted if a patient registered at the clinic calls for an ambulance or is admitted to hospital. There is a live link to the local Heartlands Hospital, where the clinic’s own team of therapists and paramedics see patients face-to-face on the wards and liaise with hospital staff to try to get them home.
“Our job is to identify which patients will benefit from our help,” says nurse Dani Fullerton. “It’s so different from anything I have done before.”
Tackling loneliness to save money
One issue the neighbourhood teams are honing in on is loneliness – they have identified this as a way to keep down hospital numbers.
Government commissioned research published in 2020 suggests the cost of severe loneliness to be more than £9,500 for each person in that category, due to the combined impact on wellbeing, health, and work productivity.
So, at the centre, local neighbourhood teams plan intense support for the most vulnerable residents, knitting together not just what the NHS and council provide, but what charities can offer too.
“We have patients going to GPs and A&E basically because they are lonely,” says Christine Francis, who is employed as a ‘social prescriber’. Her job is to help find new activities and groups for the lonely and then accompany them until they are settled.
“The NHS cannot solve [loneliness]. But I can link patients in with befriending services or, if they can get out and about, local groups such as knitting groups or organised walks.”
Ms Francis also works with groups who can help with house cleaning and tackle other issues associated with poor mental health, such as hoarding.
At present some doubt there is enough robust evidence from the research to show the effectiveness of social prescribing. The neighbourhood team is adamant their approach is making a difference, however, based on what they’ve seen first-hand.
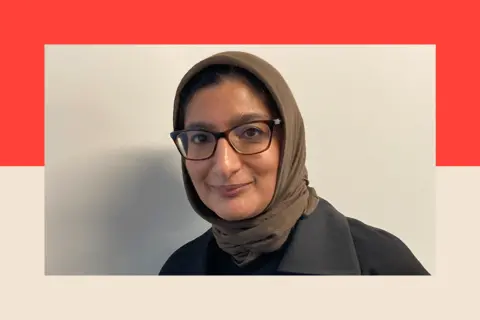
Hamzisah Aslam, an occupational therapist at Birmingham Council, recalls visiting one patient with health and alcohol problems, whose home was littered with cardboard boxes and rubbish. The visit, also attended by a GP, mental health professional and social prescriber, lasted more than an hour.
“Afterwards, we had a five-minute debrief and drew up a plan and it was actioned the next day – you would never be able to do that if we were all working individually.”
Some GPs I spoke to have also observed a positive impact. Dr Subeena Suleman says the neighbourhood team worked with two patients from her practice who were frequent visitors because of their range of health and social issues. An estimated 100 appointments at the GP surgery were freed up over six months.
“It meant we had more time for other patients,” says Dr Suleman. “We even started offering longer appointments of up to 30 minutes for those that need it.”
In the first 12 months since Washwood Heath began operating, GP visits among the local population supported by the centre fell by 31%, A&E attendances by 20% and admissions to hospital by 21%.
However, there is not yet robust evidence to quantify how much more efficient the new model would be if expanded across the city.
The knock-on effect for hospitals
The most recent addition to the centre is an emergency service for patients with respiratory illness that opened in December to address the fact that around 40% of admissions to the nearby Heartlands Hospital related to lung and breathing conditions.
So far the service, which is staffed by UHB respiratory specialist nurses and doctors, has taken in 670 patients. Christopher Thomas is one of them. He used to be a builder and worked with asbestos. Now 77, he has chronic obstructive pulmonary disease, which he believes has links to his job.
Recently, he went to hospital after coughing up blood, and was told he had pneumonia – but rather than being kept in hospital, he was discharged into the care of Washwood clinic’s respiratory service.
This, he says, worked far better for him. “I was able to stay at home to rest and take my medications and I can just ring the team at Washwood if I have any concerns.”

Respiratory medicine consultant Dr Rifat Rashid is also positive. “Here we can see and test patients quickly – there are not the delays we have in hospital waiting for results.”
But there are broader benefits for the hospital too in her view – she says GPs are starting to refer their patients directly to Washwood Heath and ambulances are also now bringing patients to the centre rather than the hospital.
Despite the benefits of fewer admissions, ultimately hospitals are no less full – while fewer people in the Washwood area are being admitted, patients from elsewhere have filled the beds.
The model is being expanded across the city – the aim is to have a network of six community hubs and 25 to 30 integrated neighbourhood teams, covering Birmingham’s population of 1.4 million people.
Not every centre will be identical. For example, in the north of the city, there might be a focus on helping with frailty to support the older, more affluent population demographic.
 Getty Images
Getty ImagesThere are of course costs – these are estimated at less than £100,000 as the six hubs as the centres will use existing buildings and redeployed staff.
Richard Kirby thinks the model could easily be replicated nationwide. “We believe this is the right model,” he insists.
But there is a catch. As he puts it, “It only works when the whole system buys into it.”
Tight budgets and a ‘cynical’ sector
Part of the problem with making the whole system buy into it is money. Ruth Rankine, an NHS Confederation primary care director, believes that during times, such as now, when money is tight, collaboration generally becomes harder.
“People are too focused on their budgets and making sure it goes on where they immediately need it,” she says.
But clinics like Washwood Heath require collaboration and pooling resources.
The other issue, she argues, is that the hospital sector has, in places, “been a bit cynical”. “The problem is that it takes time to get results – you need to invest in front and then it can be years before it has an impact.”
Another concern is around finding suitable premises. In Birmingham, officials I spoke to acknowledged they were lucky to have a network of large health centres (as they were beneficiaries of a short-lived finance programme launched in the 2000s to improve community NHS buildings) but many other places around the country do not.
This is a concern for Dr Richard Vautrey, a GP from Leeds who has been involved in national NHS politics since the early 2000s in his role as a British Medical Association negotiator and, more recently, as president of the Royal College of GPs.
“There just isn’t enough of the right premises,” he argues. “In many places, GPs and community colleagues cannot work side-by-side because the buildings are too outdated and cramped.
“We’ve had all the talk over 40 new hospitals, but where are the 1,000 new neighbourhood clinics?”
Political pressure and short-term thinking
There are deeper rooted political pressures too that make a nationwide rollout of centres like those in Birmingham a challenge.
Even though the work in east Birmingham ticks a lot of the boxes set out by independent peer and NHS surgeon Lord Darzi in his report for the government last autumn, after being commissioned by Wes Streeting, this is not the first time such calls have been made. Lord Darzi himself set out similar goals in a report for the Blair government in 2007.
Ms Rankine has had a front-row view of this. She worked for the Department of Health and NHS executive for more than a decade from the mid-1990s. “We’ve been talking about this for 20, 30 years, but failed to achieve it on any sort of scale.”
And today, there are a series of contradictory priorities facing the NHS. Often it is those considered the most pressing that are addressed first.
Hugh Alderwick, Director of Policy at the Health Foundation think-tank, who advised Labour in opposition, points out that the big focus is on hitting the 18-week hospital waiting time targets.
“It’s pulling in the opposite direction of this ambition to move care out into the community,” he observes.
So can the government really reshape the NHS into a neighbourhood health service? Dr Vautrey, for one is optimistic.
“It can,” he says. “But it will take determination, effort – and money.”
Top picture credit: Getty Images
BBC InDepth is the home on the website and app for the best analysis, with fresh perspectives that challenge assumptions and deep reporting on the biggest issues of the day. And we showcase thought-provoking content from across BBC Sounds and iPlayer too. You can send us your feedback on the InDepth section by clicking on the button below.

















Leave a Reply