March 18, 2024 – When Ken Aaron, 51, woke up from his first-ever colonoscopy last February to his doctor mouthing the words “we found a tumor,” there was no one more surprised than he was. The married father of two had some very mild GI discomfort before he booked the scan, but, besides that, there was nothing significantly amiss with the writer, an avid hiker and skier who lives in the Adirondacks.
“If I ate a fried meal, I’d feel blah,” he said. “It was more like ‘I don’t think I want that hamburger today – I don’t feel like it will sit well,’ but I don’t even know if those symptoms were related to my cancer.”
As Aaron absorbed the news that he had stage II colorectal cancer – and got over the shock of the diagnosis – he quickly realized that he would need to be his own advocate. At first, this took the form of gathering information, including a list of all the people he went to college with who became doctors.
Next, he put his case through a journalistic lens. He had no idea at the time how important this would be or that it would lead him to the frontiers of cancer science and unlikely recovery.
“I treated my diagnosis like I was doing research for a story I was writing, but the story was myself,” he said. “I started thinking: What sources do I need to talk to, what facts could I establish about my disease, and what decisions do I need to make immediately.”
Aaron isn’t alone in facing this diagnosis. Colorectal cancer is the third most common cancer diagnosed in men and women in the U.S., according to the American Cancer Society. And the number of people under the age of 50 being diagnosed with the disease has been on the rise since the 1990s – though experts aren’t sure why.
Aaron’s first option: Surgery at his local hospital to remove the mass. And at first, this made sense to him.
“When you get a cancer diagnosis, your instinct is ‘get it out of me,’” he said, adding that he and his wife also thought it would be smart to reach out to a doctor friend first. “She told us we’d be crazy not to go to a dedicated colorectal cancer care center where this is all they do.”
With that advice in mind, Aaron began cold-calling cancer centers near his home, including the University of Vermont Cancer Center, the Dana-Farber Cancer Institute in Boston, and the Memorial Sloan Kettering Cancer Center in New York City.
“I knew no one – I couldn’t drop any names – I just called Sloan Kettering’s 800 number,” he said, adding that right away, he was scheduled for an appointment at one of their New Jersey locations. “Their only questions: Do you have a diagnosis and do you have insurance. I had the right answer to both.”
An Unexpected Finding
The next morning, Aaron and his wife drove the 5 hours to Memorial Sloan Kettering on what happened to be one of the snowiest days that winter. During that appointment with Michael Foote, MD, a gastrointestinal oncologist, the couple was told all the same things that Aaron’s local surgeon told him – that he would be scheduled for surgery to remove part of his colon.
But what came next was a twist Aaron never expected.
“He told me that they wanted to look at the biopsy taken during my colonoscopy to see if I had a certain genetic deficiency that might qualify me for immunotherapy,” he said. “They told me that if I did, that would be like winning the lottery.”
When his doctor called days later to say that, yes, his tumor had a specific genetic makeup known as mismatch repair-deficient (MMRd) (present in 5% to 10% of all rectal cancer patients), he was floored, because this meant he might qualify for a cutting-edge immunotherapy clinical trial to try to shrink it – or have it disappear entirely – without chemotherapy, radiation, or surgery.
“We got so excited when we got Ken’s results,” Foote said. “In our clinical trial, we knew that the tumors in 100% of the rectal cancer patients who had immunotherapy disappeared, so we had expanded the trial to other types of cancer, including colon cancer. We thought he would be a good candidate for the trial.”
But first he would need a PET scan to make sure his tumor hadn’t metastasized. This, too, prompted another shocking finding. During the scan, one of his lymph nodes lit up, so he was scheduled for a biopsy right away. The finding: Aaron also has low-grade follicular lymphoma – that had nothing to do with his colon tumor.
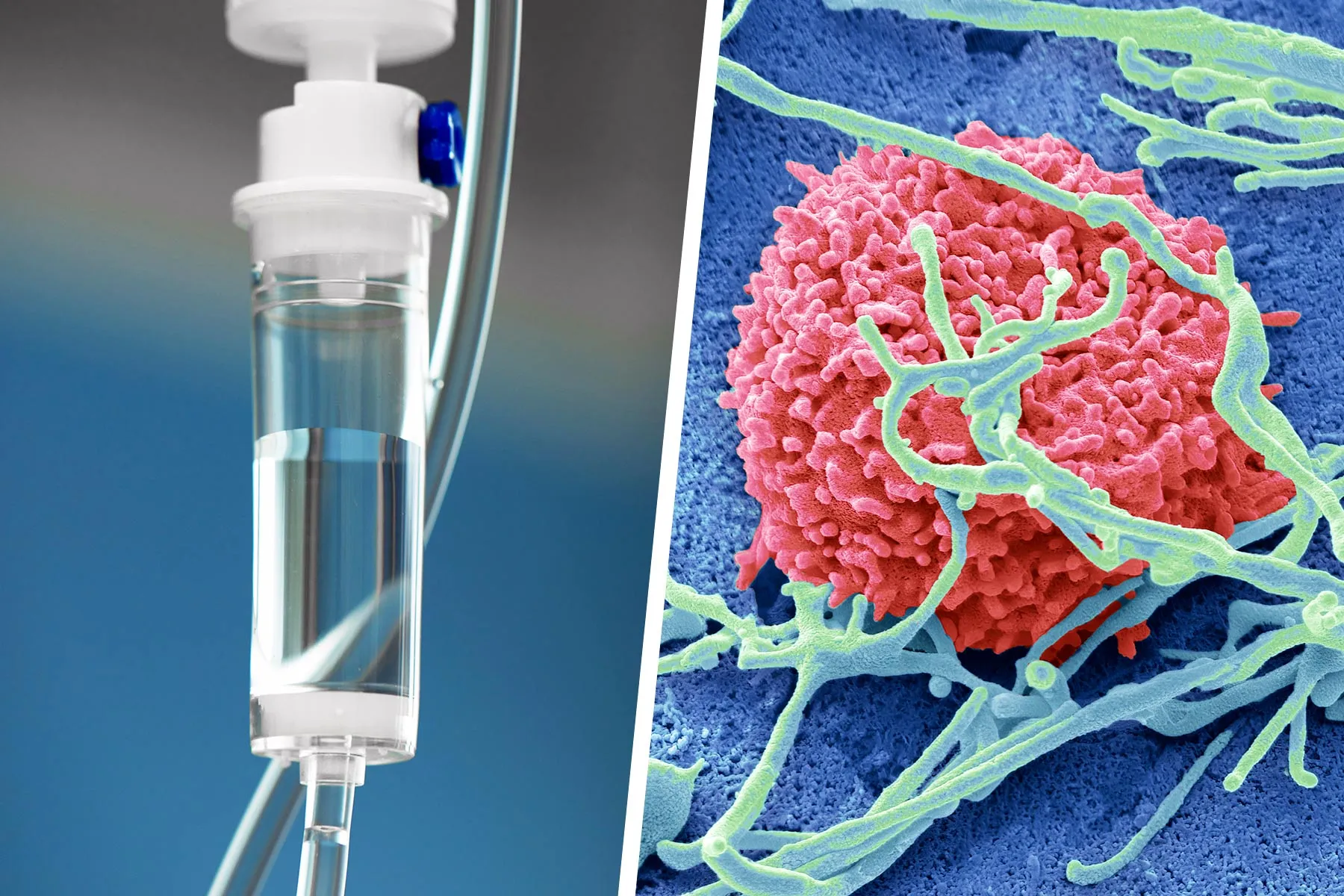
Because Aaron now had two cancers, he no longer qualified for the clinical trial, but that didn’t stop his team from starting him on pembrolizumab (Keytruda) instead of dostarlimab (Jemperli), the drug being used in the trial.
“This was an additional complication, as lymphoma is a cancer of the immune system and we would be using immunotherapy to treat Ken’s colon cancer,” Foote said. “It wasn’t clear at first how effective it would be, but we decided to try it.”
In April, Aaron had the first of his nine immunotherapy IVs of Keytruda, 2 ounces at a time, given every 3 weeks. Aaron had virtually no side effects, except that his existing gout got worse.
“This isn’t like chemo,” he said. “I can drive to the cancer center and back and even go skiing or hiking the next day.”
A Potential Bump in the Road – and Then a Miracle
After the fifth treatment, Aaron had another PET scan and another colonoscopy. It showed that he was making progress, but it was slower compared to other patients in the clinical trial.
“That was frustrating,” he said. “But my oncologist said that he thought my lymphoma might be the reason – they were giving me drugs to kick my immune system into gear, but lymphoma is a cancer of the immune system, so he explained that it might be tugging in the opposite direction a bit.”
It was only after his seventh treatment, colonoscopy, and another scan that a miracle happened: There was no sign of the tumor, and the biopsy came up clean.
“There was no cancer detected, and there was only scar tissue where the tumor was,” he said. “It was a miracle – I still can’t believe I’m saying this out loud.”
As per protocol, Aaron completed his treatment and had his final treatment in September. He has since had two PET scans, with another coming in June. He will get colonoscopies every 4 months for the foreseeable future.
“You’re never really done – it’s just a new phase,” he said. “This is why they have support groups for cancer survivors. It’s not because you sit around and exchange high-fives. You’ve been on a war footing, and now you’re not, and you have a little PTSD. It’s definitely a traumatic experience.”
Aaron remains the de facto organizer of an online support group with his fellow Sloan Kettering patients.
“We’re still helping each other,” he said. “I’m still scheduling our Zooms every other Tuesday at 3 p.m. We need each other, and I know it helps all of us to talk to each other about what we’re going through.”
Ultimately, Aaron said, he’s walked away from this situation with a new philosophy.
“The answer is to extend empathy to everybody you meet and to do it perhaps more than I was doing it every day,” he said. “It’s not necessarily because you never know what somebody has going on. That’s true. But, even more than that, if you extend grace and somebody else does it in turn, the world becomes a better place.”
Aaron’s Tips for Advocating for Yourself
Make Sure Your Doctor Listens to You
“If you think something is wrong, get an answer,” he said. “You know your body best. If you feel like something’s not right, don’t let it go. If your doctor isn’t responsive, find another. Before I was diagnosed, I’m glad to say my primary care doctor was very attentive to my concerns, even though they were subtle; I’m still not sure they were related to my cancer. But I know others whose initial concerns were ignored.”
Escalate the Situation Right Away
“Find an institution or hospital that specializes in your cancer and go there. I wanted to be the most boring case my doctor saw all week, not the most interesting.”
Find the Best ‘Cancer Machine’ Near You
“In choosing to go to [Sloan Kettering], I felt like I engaged a ‘cancer machine,’” he said. “By becoming a patient there, I enlisted countless advocates on my behalf, an entire medical team steeped in the latest advances. I almost certainly wouldn’t have been put on the same treatment protocol if I didn’t go there.”
Let Your Doctors Take Care of You
“Cancer throws a lot of questions at you that can be really hard to answer, and while you want to advocate for yourself, it’s hard to know if you’re making the right decision,” he said. “Google only goes so far, but by going to a place like [Sloan Kettering], it was a relief to know that even if things went sideways – and they certainly could have as there are no guarantees with cancer – I at least took the ‘what if’ off the table. And at a time when it’s really the uncertainty that’s the hardest thing of all, it’s comforting to know you’ve done that for yourself.”
https://img.lb.wbmdstatic.com/vim/live/webmd/consumer_assets/site_images/articles/health_tools/questions_to_ask_doctor_about_egfr_positive_nsclc_slideshow/1800ss_science_source_rm_combination_chemo_and_immunotherapy.jpg
2024-03-18 19:53:25