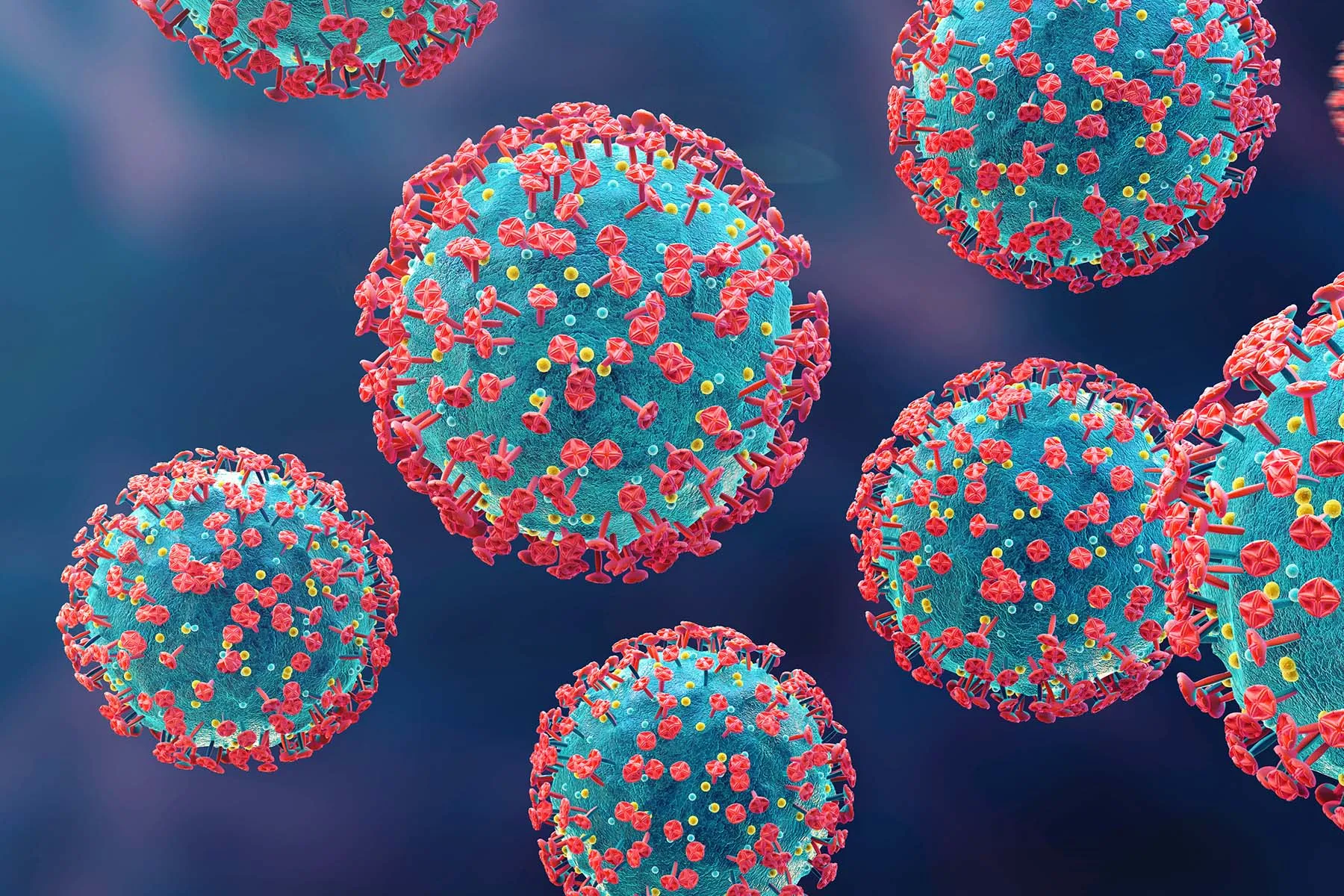
Sept. 25, 2023 — As we continue to live with COVID-19, patients and doctors will learn more about the reasons infections can range from asymptomatic to very serious. Many researchers and doctors believe inflammation is the cause of severe COVID. This is due to the virus causing a “cytokine storm” that can adversely affect the organs in a patient’s body, including the heart and lungs.
New research from Northwestern University and the University of Wisconsin, however, is pointing to bacterial pneumonia as the cause of many severe COVID deaths. Deceased COVID patients studied were not shown to have experienced inflammation at all. Instead, the researchers, using machine learning to analyze data, found that half of the severely ill COVID patients who required a ventilator had bacterial pneumonia as a secondary infection. They did not find evidence of a cytokine storm in these patients; instead of dying from organ damage or failure due to COVID, they died of pneumonia.
“Critically ill patients who recovered from pneumonia were more likely to live,” said Benjamin D. Singer, MD, senior author of the study, professor of pulmonary medicine, and a Northwestern Medicine pulmonary and critical care doctor in Chicago.
Other researchers don’t debunk the idea of cytokine storms in COVID, however. Cytokines are chemicals that are released when a person’s immune system overreacts to an infection. Too many cytokines are toxic and can cause organ failure. In COVID-19, cytokines have been thought to release inflammation that can circulate through the body and cause death.
A new study from CSIR-Institute of Microbial Technology in Chandigarh, India, and M. M. Engineering College in Ambala, India, for example, found that controlling this inflammatory factor is essential in order to treat COVID. Italian researchers further find that hyperinflammation plays a definite role in severe illness in COVID patients.
Additional new research does show that specific bacteria can cause negative outcomes for COVID patients. A study from the New York University Grossman School of Medicine found that bacteria from the gut may move into the blood of patients with severe COVID. “Bacteria circulating in the blood can accelerate complications in these COVID patients,” said study co-author Jonas Schluter, PhD of the Institute for Systems Genetics and assistant professor of microbiology at NYU Grossman in New York City.
Can these findings affect any patient who is diagnosed with COVID-19 and may be at high risk for complications? Potentially, yes. A very important aspect of the Northwestern study is that it highlights the importance of screening susceptible COVID patients for pneumonia as soon as possible. The good news: Patients who test positive can immediately talk to their doctors about their risk factors and get the treatment they need to prevent serious illness.
Who Is at Risk for Severe COVID?
The CDC reports that anyone who is unvaccinated is at risk for severe COVID. Other factors include:
- Being over age 50, especially over age 65
- Having underlying medical conditions including asthma and other respiratory conditions, diabetes, heart disease, HIV, kidney disease, liver disease, having a suppressed immune system, and obesity.
- Being pregnant
- Being physically inactive
- Being a smoker
What Symptoms of COVID Are Emergency Warning Signs?
According to the CDC, symptoms of COVID that can range from mild to severe include:
- Fever
- Chills
- A cough
- Shortness of breath or any difficulty breathing
- Tiredness
- Muscle aches
- Body aches
- A headache
- Loss of taste
- Loss of smell
- A sore throat
- Congestion
- Runny nose
- Nausea
- Vomiting
- Diarrhea
The following symptoms indicate a potentially more serious or critical progression of COVID-19:
- Difficulty breathing
- Chest pain pain
- Chest pressure
- Confusion
- Trouble waking up
- Trouble staying awake
- Pale, gray, or blue-colored skin, lips, or nail beds
Anyone experiencing any or all of these symptoms should call 911 right away and explain that this is a confirmed or possible case of COVID.
How Is Severe COVID Treated?
If a patient tests positive and has risk factors, their doctor may prescribe one of three drugs to keep the illness from progressing: molnupiravir, Paxlovid, or remdesivir. If a patient is hospitalized, additional drug therapy that reduces inflammation may be given, as well as blood plasma therapy.
Patients will also be treated for any other infections they have, which is why it’s important to let health care providers know about new symptoms right away.
What Can Be Done to Avoid Severe COVID-19?
First, get vaccinated and boosted. “It’s the best way to prevent the likelihood of severe illness,” Singer said. “It’s very rare to see a fully vaccinated COVID patient critically ill in the ICU.”
If a patient tests positive and has respiratory symptoms that are worsening, they should ask their doctor for a pneumonia screening. Antibiotics are often necessary to treat a co-infection, and Schluter had some unexpected but important advice: Stop eating junk food immediately. “You don’t want to eat rubbish because antibiotics and sweets do not mix,” he cautions. “Sugar from your diet, combined with antibiotics, can exacerbate damage to the organs in your body. COVID can create a forest fire in your body. Not consuming excess sugar can extinguish the flame.”
The most important things to do: Take all prescribed medication, isolate for at least 5 days, wear a high-quality N95 or KN5 mask around others, and don’t stress. Taking these steps means a patient is doing everything right, and everything possible, to have the least severe outcome with COVID-19.
https://img.wbmdstatic.com/vim/live/webmd/consumer_assets/site_images/articles/health_tools/reasons_your_viral_load_might_become_detectable_slideshow/1800ss_getty_rf_hiv_virus.jpg
2023-09-25 16:32:22