July 28, 2023 – What is the first thing that comes to mind when you hear the term “game-changer”? For two-time Olympian, three-time Women’s World Cup player, and former professional soccer player Rosie White, it’s a condition called ulcerative colitis, and it would be a takeover that neither she nor her teammates anticipated.
“I was playing collegiate soccer at UCLA and also playing for the New Zealand national team, and I started feeling symptoms during an international game,” White said. “And I just thought that I was sick, had diarrhea, or had eaten something funny.”
“There was blood in my stool, and I was like, “this is not normal; this is not something I’ve experienced before.”
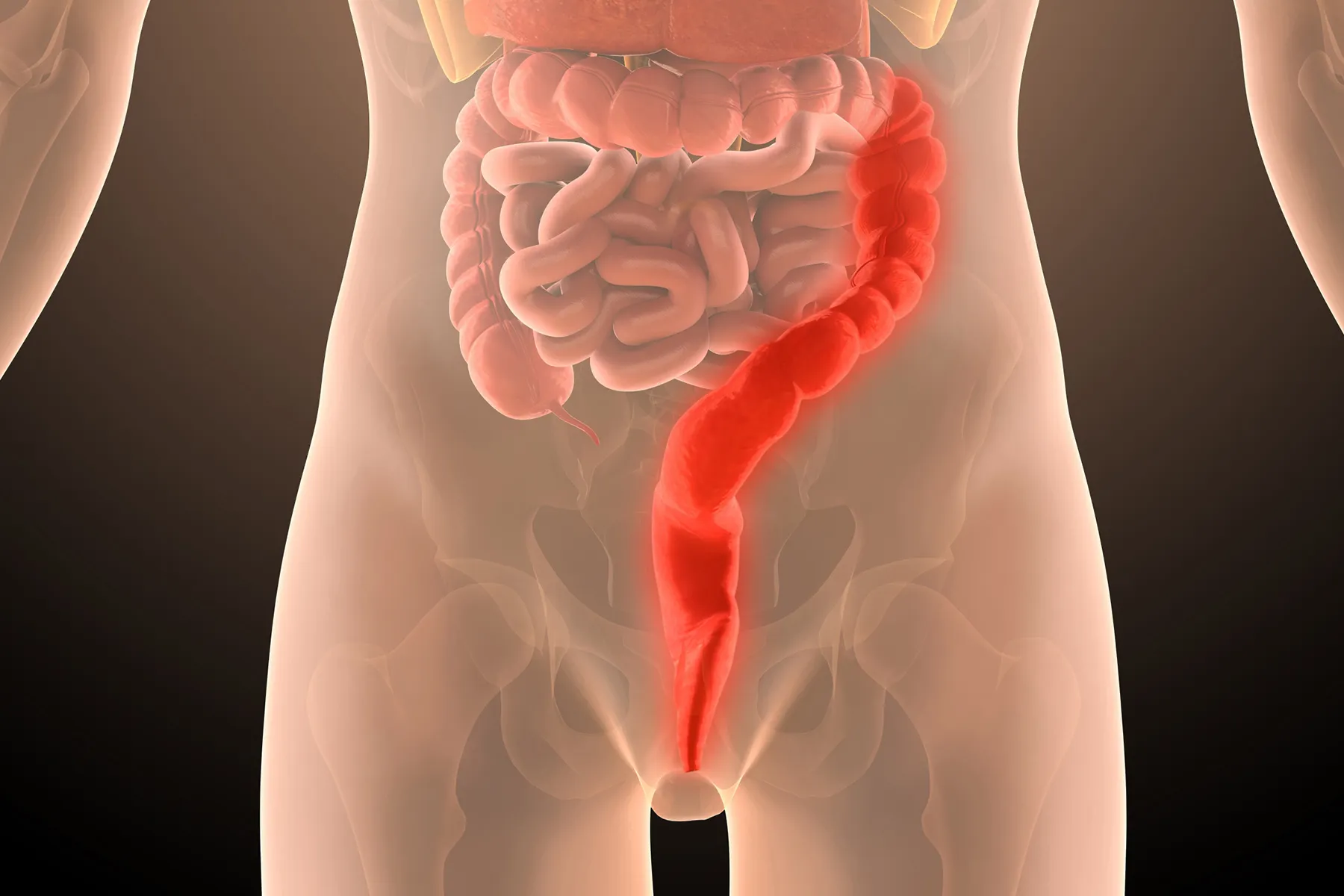
At the time, White was 19, an age when ulcerative colitis commonly emerges. The disorder is a type of inflammatory bowel disease (IBD) that causes irritation, inflammation, and holes (ulcers) in the lining of the colon. For many, ulcerative colitis stalks and colors every part of life. Symptoms, which might include severe diarrhea, bowel urgency, cramps, pain, and fatigue, can literally stop people in their tracks, or in White’s case, interrupt a pivotal 100th celebratory game intended to mark her career with the New Zealand Ferns.
“It was supposed to be a really big moment to celebrate,” White said.
Instead, “it was probably the worst I’ve ever felt playing a game of soccer before. I remember collapsing at 90 minutes, and the team doctor had to carry me off the field. I just laid in the locker room on the floor for like an hour, trying to stop the cramps in my stomach.”
Doing the Doctor Shuffle
Ulcerative colitis is a condition without an exact known cause. Although researchers continue to make strides in their understanding of it, diagnosis can be difficult.
“The general idea is that this is a condition with a genetic predisposition, but genetics alone don’t explain it because it does miss many generations,” said Victor Chedid, MD, a gastroenterologist specializing in IBD at the Mayo Clinic in Rochester, MN. “Environmental factors are important components as well; I wouldn’t discount diets and changes in diet, we know that a lot of processed foods and sugars can be pro-inflammatory. And I wouldn’t discount stress, which can trigger or increase the inflammatory burden.”
Along with general symptoms like diarrhea and cramps, these things make a delayed diagnosis more likely.
Chedid noted that it can often take patients months, if not years, to finally land in the right doctor’s office and get the right diagnosis, an experience that White knows all too well.
“I ended up seeing a number of different doctors to talk about what was going on,” she explained. “I remember getting really frustrated because I think I saw about two or three different GPs because I was bouncing around, traveling with the New Zealand team. And all of them were like, ‘Everything seems healthy,’ and they weren’t concerned at all.”
It wasn’t until she saw yet another doctor back at school in Los Angeles, who finally recommended she see a specialist, that she finally received a diagnosis and medication to help control her symptoms.
A Subject No One Wants to Discuss
Like many ulcerative colitis patients, White recalled that for a long time, she was “super embarrassed” about her condition.
“It’s a really difficult thing to talk about. Nobody wants to talk about their poop and their bowel movements,” she said, also noting that at first, she spent a lot of time putting out fires each time her condition flared.
A key missing piece of the puzzle was education. Not only did she find herself looking in all of the wrong places for information, but in hindsight, she wishes that she had had more people around her that knew what was going on to support her.
“I didn’t talk about it for 5 years. And what I learned the hard way is that the longer you wait, the worse your symptoms get, and they’re harder to control. And I ended up in the hospital for a week and a half because I didn’t seek help quick enough,” White said.
Her advice to others?
Seek a website that has really good information, find treatment options that support your lifestyle, and get your family, friends, and support network on board and aligned.
The Role of Diet
“When I am thinking about the tools I’m providing to patients to help and empower them to get their disease in remission, medicine is only one; another is that we have to get you on a good nutrition or better, healthy eating program,” said Chedid.
Kelly Issokson, a registered dietitian and certified nutrition support clinician who specializes in GI issues at Cedars-Sinai Medical Center in Los Angeles, said one of the first questions patients ask is what they can eat.
“Nutrition is so important for the management of IBD,” she explained. “It helps improve response to medications that help control IBD, and … in disease management, there are certain diets or food components that we can recommend to decrease inflammation.”
Fortunately, White was on the right diet and nutrition track from the start. Although her journey included a brief stint with a doctor-recommended vegetarian diet, and included trying “every diet in the book,” as a professional athlete, she had long relied on whole, non-processed foods and avoided things like sugar and alcohol.
Issokson said that in general, people with ulcerative colitis should consume a diet that is rich in variety, including a lot of food groups and sources, like different types of fruits and vegetables and different proteins. These are parts of the Mediterranean diet that, Chedid noted, has been shown to have less pro-inflammatory food than the traditional American diet.
“There are certain things that we know about food components and how they affect ulcerative colitis in particular,” Issokson added. “We know that omega-3 fatty acids are really important to consume – not only in supplement form, but in food form because they help control disease activity as well as have an anti-inflammatory effect.”
And people should be aware of and recognize how they’re feeling.
“People with active disease are going to have different nutritional needs than people whose disease is in remission,” Issokson said. For example, people might have less of an appetite or certain GI symptoms and might do better with small, frequent meals to decrease urgency and diarrhea.
And for people with specific food triggers such as lactose, a sugar that is found in dairy products, Issokson counsels patients to choose plain yogurt, aged cheeses, or even nondairy, plant-based milk.
Other triggers might include sugary foods and beverages (which can worsen urgency and diarrhea) or certain medications like prednisone (which can increase blood sugar).
Stress and Inflammation
There’s a direct link between mental health and inflammation in the gut, a key reason why addressing mental health is an important part of the ulcerative colitis toolbox.
Laurie Keefer, PhD, a psychologist specializing in IBD at Icahn School of Medicine at Mount Sinai in New York City, said, about a quarter of ulcerative colitis patients have depression and about a third have anxiety, often together and within 1 or 2 years of diagnosis. Both either precede or develop as the result of things like isolating oneself from family and friends, or avoiding travel or leaving one’s home for fear of having an accident.
“I always describe it like a background app that tracks your location, even if you don’t need it to. And that leads to fatigue,” she said.
“I think that it’s a huge, huge part of this disease,” said White of the mental health connection. “Physically, your body’s going through a lot. But also emotionally, the symptoms themselves cause a lot of stress because you’re always worried about where the bathroom is, when you’re going to need to go, things like that.”
For White, being open and honest with her family, friends, and others in her circles, and having a good relationship with her doctor, have helped remove the stress barrier. These steps are an important part of what Keefer described as acceptance-based work.
“We do a lot with self-compassion and gratitude, tell our patients to give themselves grace, treat themselves like they would a friend who was telling them about the same symptoms,” Keefer said. “For symptom management, there’s more of a cognitive behavioral component, which [helps] people ‘de-catastrophize’ the significance of the events; we try to shift the positive and make people feel more optimistic.”
Speaking of optimism, White is the epitome, and her outlook is well, rosy. Now age 30, she’s traded the soccer field for the television microphone, is a spokesperson for Bristol-Myers Squibb, and has her ulcerative colitis toolbox down pat: medication, support, and a good relationship with her doctor.
On or off the field, she’s definitely become the version of herself that she’s long strived for.
“Learning to be the best advocate for yourself is key,” she said.
https://img.wbmdstatic.com/vim/live/webmd/consumer_assets/site_images/articles/health_tools/uc_and_malnutrition_slideshow/1800ss_getty_rf_ulcerative_colitis_illustration.jpg
2023-07-28 18:23:07