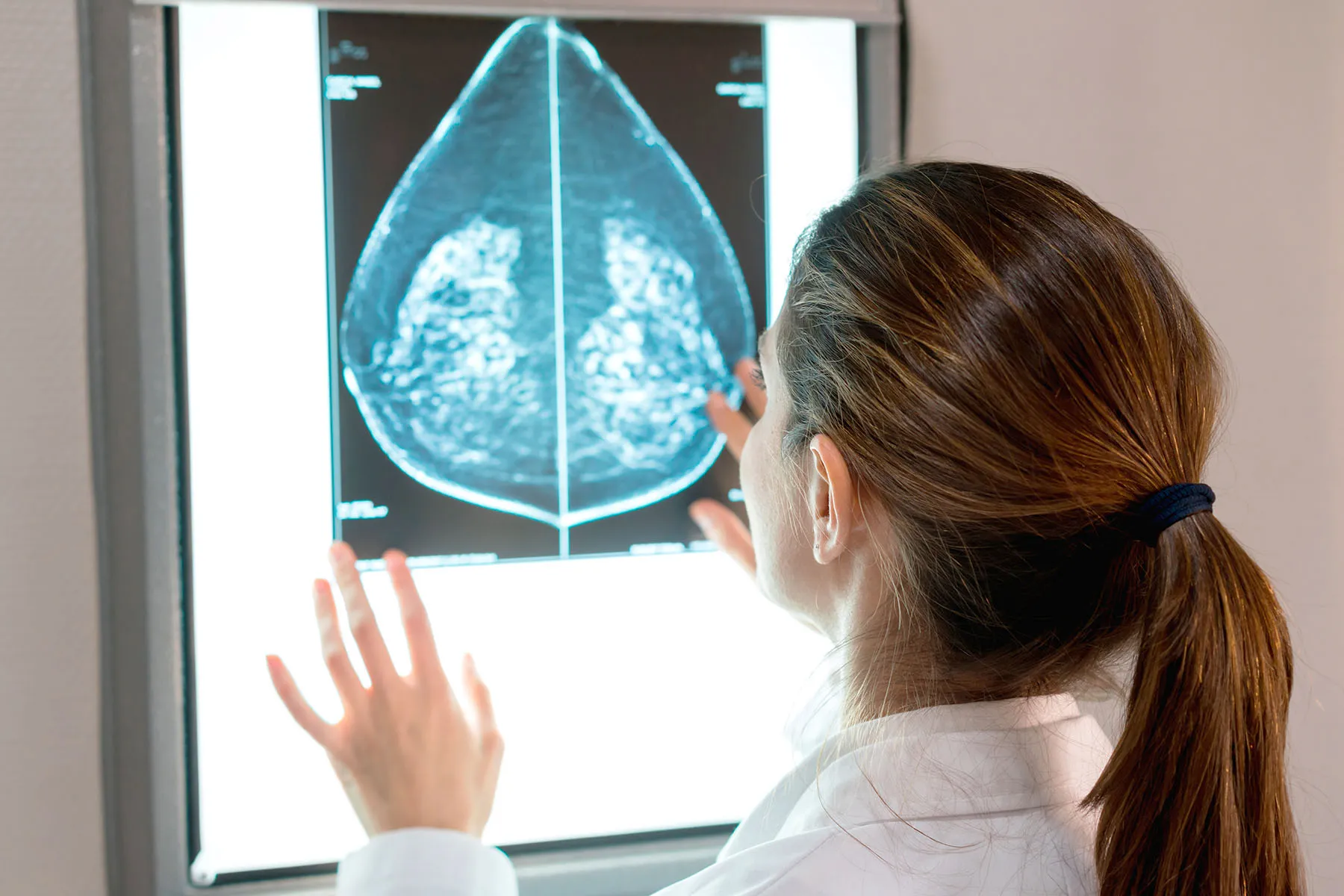
May 9, 2023 – Women should start being screened for breast cancer at age 40 instead of waiting until 50, the U.S. Preventive Services Task Force said Tuesday in a draft recommendation statement.
The critical change in age for mammograms also includes the recommendations for screening every other year and sets a cutoff age of 74.
The task force’s ratings system shows strong confidence in the evidence for benefit from the changes, meaning that doctors should encourage their patients to get screened as appropriate.
The influential federal advisory panel last updated these recommendations in 2016. At the time, the task force recommended routine screening mammograms starting at age 50.
In the 2016 recommendations, “we felt a woman could start screening in her 40s depending on how she feels about the harms and benefits in an individualized personal decision,” said task force member John Wong, MD, chief of clinical decision making and a primary care doctor at Tufts Medical Center. “In this draft recommendation, we now recommend that all women get screened starting at age 40.”
Two major factors prompted the change, Wong said. One is that more women are being diagnosed with breast cancer in their 40s. The other is that a growing body of evidence shows Black women get breast cancer younger, are more likely to die of breast cancer, and would benefit from earlier screening.
“It is now clear that screening every other year starting at age 40 has the potential to save about 20% more lives among all women and there is even greater potential benefit for Black women, who are much more likely to die from breast cancer,” Wong said.
The American Cancer Society called the draft recommendations a “significant positive change,” while noting that the task force recommendations only apply to women at average risk for breast cancer.
The American College of Radiology already recommends yearly mammograms for average-risk women starting at age 40. Its latest guidelines on mammography, published May 3, call for women at higher-than-average risk for breast cancer to undergo a risk assessment by age 25 to determine if screening before age 40 is needed.
When asked about the differing views, Debra Monticciolo, MD, division chief for breast imaging at Massachusetts General Hospital, said annual screening would save more lives than the every-other-year approach backed by the task force. Monticciolo also said that the available scientific evidence supports earlier assessment as well as earlier-than-age-40 screening of many women, particularly Black women.
“These evidence-based updates should spur more-informed doctor-patient conversations and help providers save more lives,” Monticciolo said in a news release.
Insurance Access
Typically, upgrading a task force recommendation from a grade of C to B leads to better access and insurance coverage for patients. The Affordable Care Act requires insurers to cover the cost of services that get A and B recommendations without charging copays — a mandate intended to promote greater use for highly regarded services.
But Congress created a special workaround that effectively makes the Affordable Care Act mandate apply to the 2002 task force recommendations on mammography. In those recommendations, the task force gave a B grade to screening mammograms every 1 or 2 years starting at age 40 without an age limit.
Federal lawmakers have sought to provide copay-free access to mammograms for this entire population even when the task force recommendations in 2009 and 2016 gave a C grade to routine screening for women under 50.
Still, “it is important to note that our recommendation is based solely on the science of what works to prevent breast cancer and it is not a recommendation for or against insurance coverage,” the task force acknowledged when unveiling the new draft update. “Coverage decisions involve considerations beyond the evidence about clinical benefit, and in the end, these decisions are the responsibility of payors, regulators, and legislators.”
Uncertainties Persist
The new draft recommendations also highlight the persistent gaps in knowledge about the uses of mammography despite years of widespread use of this screening tool.
The updated draft recommendations emphasize the lack of evidence to address major areas of concern related to screening and treating Black women, older women, women with dense breasts, and those with ductal carcinoma in situ (DCIS), which is also called stage 0 breast cancer.
The task force called for more research to address the underlying causes of elevated breast cancer death rates among Black women.
“Nearly half of all women have dense breasts, which increases their risk for breast cancer and means that mammograms may not work as well for them. We need to know more about whether and how additional screening might help women with dense breasts stay healthy,” the task force said.
The task force also called for more research on approaches to reduce the risk for overdiagnosis and overtreatment for breast lesions, such as DCIS, which are identified through screening.
The task force will accept comments from the public on this draft update through June 5.
https://img.webmd.com/vim/live/webmd/consumer_assets/site_images/articles/health_tools/who_are_the_members_of_your_breast_cancer_care_team_slideshow/1800ss_getty_rf_gynecologist_looking_at_mammogram.jpg
2023-05-09 19:33:18